PCR Lab: How to prevent false positives in COVID-19 nucleic acid testing?
Nucleic acid testing is the "gold standard" for COVID-19 testing. Real-time fluorescent quantitative RT-PCR is a common method for clinical testing. With the widespread use of this method in laboratories at all levels, false positives in clinical testing of large quantities of samples cannot be ignored. The problem. In simple terms, the false positive of real-time quantitative PCR means that a fluorescent signal appears in a sample that should not have a fluorescent signal, which leads to a misjudgment of a positive result.
The main reasons for false positives are as follows:
1. Inappropriate primer design: The selected amplified sequence has homology with the non-target amplified sequence, so when performing PCR amplification, the amplified PCR product is a non-target gene sequence. However, in clinical practice, due to the basic use of finished kits, improper primer design will generally not occur, but there are still non-specific amplification phenomena in the reagents of individual manufacturers. It is recommended to perform performance evaluation and comparison screening before use.
2. Cross-contamination of target sequence or amplification product. There are two reasons for this contamination:
1. It is the cross-contamination of the entire genome or large fragments that leads to false positives.
2. It is the contamination of small fragments of nucleic acid in the air. Although these small fragments are shorter than the target gene sequence, they have a certain degree of homology. After being spliced with each other and complementary to the primers, PCR products can be amplified, resulting in false positives. Under the premise of standard operation, the second situation should be avoided as much as possible.
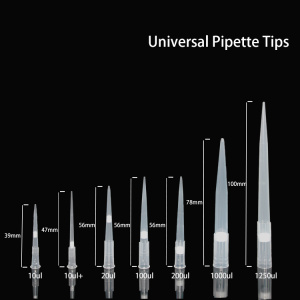
3. Cross-contamination between specimens: The main contamination of specimens is that the container for collecting the specimens is contaminated, or when the specimen is placed, it is leaked out of the container due to loose sealing, or there are specimens on the outside of the container, causing mutual cross-contamination; the sample nucleic acid template is being extracted During the process, due to the contamination of the suction gun, the contamination between the specimens; some microbial specimens, especially viruses, can spread with aerosols or form aerosols, resulting in mutual contamination.
4. The contamination of PCR reagents: mainly due to the contamination of the PCR nucleic acid template by the sample gun, container, double distilled water and other solutions during the preparation of PCR reagents.
V. Contamination of cloned plasmids in the laboratory: The positive control in the kit participates in the nucleic acid extraction process and causes cross-contamination. In order to monitor the quality of the nucleic acid extraction process, some kits require the positive control in the kit (false virus containing the target gene) ) Perform nucleic acid extraction together with the sample. Due to processes such as heating and vibration, the aerosol may contaminate the extractor during the operation of the automated nucleic acid extractor. Some laboratories may store the extracted nucleic acid sample plate with membrane for amplification, and cross-contamination may be caused when the membrane-sealed sample plate is opened again. Therefore, it is not recommended to seal the nucleic acid of the extracted sample and save it. It is best to test it immediately. At the same time, each batch of the extracted instrument should be wiped with 75% alcohol.
When the PCR experiment results show false positives, we often consider whether the template is contaminated by primers, reaction solutions, pipettes, etc., and then we need to check one by one, which is time-consuming and labor-intensive. In fact, the most common cause of this phenomenon is nucleic acid aerosol. Centrifugation in a centrifuge, vigorous shaking of the reaction tube, opening of the PCR cap, repeated pipetting of the pipette, etc. will cause friction between the air and the liquid surface, which will generate nucleic acid aerosols, which is in the laboratory (or in the pipette cavity) There are small particles containing nucleic acid fragments of different lengths. These small particles settle into the sample and finally amplify a false positive fluorescence curve.
It is conceivable that these small nucleic acid particles will also fall on the experimental table, PCR machine, pipette, tip box, etc. If we do not pay attention, these small nucleic acid particles will accumulate over time, when the nucleic acid in the laboratory When the concentration of aerosol reaches a certain concentration, it will cause laboratory pollution and cause false positives in PCR test results.

Then we should avoid the generation of nucleic acid aerosol pollution in the following aspects in our daily work:
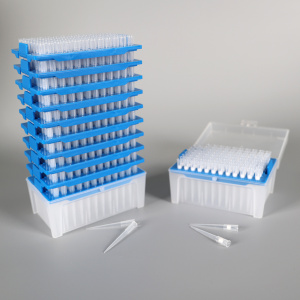
1. Reagents should be aliquoted in advance: the reaction solution should be aliquoted as much as possible to avoid multiple use, and the primers and probes should be diluted to a certain concentration and then aliquoted to ensure that there is a backup to prevent the entire tube from being annihilated after contamination;
2. The water needs to use RNase-free deionized water, you can buy special water from the reagent company;
3. Be careful and gentle when adding samples to prevent the template from being sucked into the sampler or spilled out of the centrifuge tube. The order of sample addition is to add the template last.
4. All centrifuge tubes and sample pipette tips should be used for one time. If necessary, the reaction tube is irradiated with ultraviolet light before use to destroy the existing nucleic acid.
5. After the machine is running, the PCR product should not be discarded casually when taking out the PCR product. It should be wrapped in plastic gloves or other knots and then thrown into the trash can.
The following aspects should be paid attention to in the daily management of the laboratory:
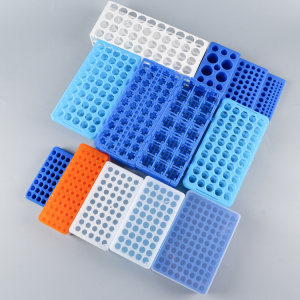
1. The laboratory should be divided into at least three areas: reagent preparation area, template preparation area, product amplification analysis area, each area is equipped with a separate pipette (each area should be in a different room if conditions permit, so as to maximize Avoid pollution).
2. The laboratory should pay attention to the wind direction and the pressure difference in each zone, and the relative pressure difference should also be the process from high to low from reagent preparation to product analysis direction;
3. Clean the laboratory regularly. Different areas have their own special wipes. Contact surfaces such as countertops, instruments, tip boxes, desktops, and the ground need to be wiped clean with different concentrations of chlorine-containing disinfectants. The surface of the instrument is 75% Wipe with alcohol, clean the dangerous area, and use full-exhaust air supply for laboratories with conditions.